



Three benefits experts recently discussed how to effectively evaluate various health offerings and their impact on ROI during the webinar, 3 Steps to Re-Evaluate the ROI of Your Well-Being Program. A central theme of the conversation was the idea that for real behavioral change, employers are seeking innovative ways to meet their population's specific needs. Gone are the days of a one-size-fits-all approach to wellness. Now there’s a significant shift toward more tailored and customized solutions.
Presenters:
Factors driving the Great Re-Evaluation. Employers are facing new challenges in the post-pandemic era, prompting a re-evaluation of health benefits programs. According to Aon's research, controlling health care costs is the top priority for employers in 2024. What’s driving costs up? Factors include inflation, advances in medical technology, expensive drugs like GLP-1s, an aging population, overuse of care services, and underuse of preventive care.
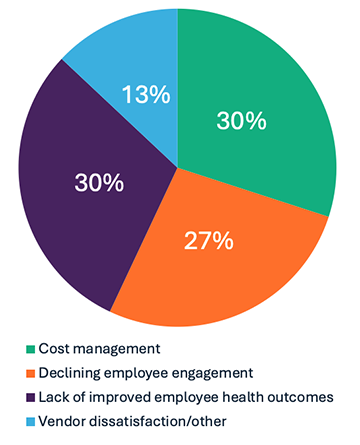
An audience poll showed a surprising three-way split. Participants were asked to identify their primary driver if they are re-evaluating their health and well-being program(s) in 2024. The answers revealed that employers are concerned equally with managing costs, declining employee engagement, and lack of improved employee health outcomes. The speakers noted that these factors are interconnected, emphasizing the need to address engagement and health outcomes to determine the cost-effectiveness of programs.
Employers’ primary drivers when re-evaluating health and well-being programs:
Evaluating ROI of health and well-being programs starts with three things:
1. Identify controllable costs. What are the cost drivers and how can we impact them? Different populations have different controllable costs. Start with condition-specific care such as cancer, cardiovascular, MSK, diabetes, and mental health, followed by specialty drugs like GLP-1s. These are all related to cost and utilization. Employers need to tackle conditions from multiple angles with such things as facilitating preventive care, assessing workplace environment and culture, and encouraging the controllable portion of that spend, with lifestyle factors and more.
2. Demand the right data from vendors. Employers should leverage data to understand areas of opportunity and impact.
— Kristen Grady, Vice President, Health Transformation Team, AonIt sounds obvious, but asking these fundamental questions to start, "What does success look like?” and “How is it measured?” are crucial to understanding what data will produce meaningful outcomes. Other questions such as, “Is the right population engaged?” and “Is the engagement sustained?” should be asked as well.
And timing is important, too. It’s not possible to get a firm grasp of success in a few months. Kristen Grady from Aon added, “Clients get so excited when they find the right partner, they implement them and everyone wants to know in two months, is it working? Behavioral change takes time. And it’s really helpful to define what will be measured in 6, 12, 18, and 36 months.” Setting clear expectations with time-based metrics over longer periods is realistic. Grady continued, “Documenting why a vendor was chosen and outlining their expectations for success is key.”
3. Respond to employee needs for meaningful engagement. Employers can offer the best program, but if employees don’t engage, then success remains elusive. Employers must balance understanding their population's preferences and needs with actual program utilization. With 3–4 generations in the workforce today, the needs of Gen Z will not be the same as the Baby Boomers. For example, Regina Ihrke from WTW said, “With Gen Z, mental health is a broken-down stigma. They see mental health and therapy as a key piece and are very open to virtual care, while Baby Boomers may be delaying retirement and have more chronic conditions.” Customizing health and well-being offerings and diving deeper into “micro-segmenting” will become necessary to meet the needs of various populations.
— Regina Ihrke, ASA, MAAA, Health, Equity and Wellbeing Leader – North America, WTWGetting employee feedback about what programs are needed is important, but many times it comes down to awareness and access. Do employees know what programs are available to them? Are they being communicated to through multiple channels, and often?
Offerings like virtual care and digital engagement have gained momentum, especially with the shift to remote work, but employers need to align offerings with the cultural and generational preferences of their workforce.
Key takeaway: The speakers highlighted the industry's move towards more integrated, customized, and personalized well-being programs, driven by a need for more measurable ROI, data-driven insights, and meaningful engagement.
